Table of Contents
Temporomandibular disorders (TMDs) are a heterogeneous group of musculoskeletal and neuromuscular conditions that involve the temporomandibular joint (TMJ) complex, including the surrounding musculature and its bony components (gnathological or masticatory system).
TMDs affect up to 15% of adults, with a maximum incidence between 20 and 40 years of age (they are twice more common in women than in men), being one of the main causes of non-dental pain in the orofacial region.
Common symptoms include jaw pain or dysfunction, earache, headache, and facial pain. The etiology of TMDs is multifactorial and includes biological, environmental, social, emotional and cognitive triggers.
Diagnosis is often based on a medical history and physical examination. Imaging can be helpful when severe malocclusion or intra-articular abnormalities are suspected.
Most patients improve with a combination of noninvasive therapies including occlusal (bite) analysis, selective grinding, professional guidance, self-care, cognitive behavioral therapy, drug therapy, physiotherapy, use of occlusal splints, and sometimes orthodontics. Initially (in the acute phase), non-steroidal anti-inflammatory drugs and muscle relaxants are recommended, which can be supplemented with benzodiazepines or antidepressants in chronic cases.
Multidisciplinary treatment that includes the participation of Physiotherapists, Psychologists, Otolaryngologists and/or Neurologists, or the intervention of other Specialist Dentists such as the Orthodontist, Prosthodontist or Maxillofacial Surgeon; it is indicated for the most complex, advanced or refractory cases. However, the first step in understanding and evaluating the different treatment options is knowing the different types of masticatory dysfunction.
Classification of Temporomandibular Disorders
Although the scientific classification is quite extensive and complex, we have tried to condense it (according to its level of severity) into only 6 groups or categories; so that it is easy to understand, limiting ourselves only to the most important ones:
1- Muscular Disorders
As a general rule, the muscles and other extra-articular elements of the masticatory system are the first affected in any dysfunction, although later their alterations usually accompany it throughout its evolution.
The most important thing is to know that muscles bother or hurt when they work too much and/or incorrectly. Simply put, overworked muscles face contraction, fatigue, and spasms.
Later, if the condition and the factors causing the disharmony are not corrected on time, they gradually affect the functioning and internal structure of the temporomandibular joint, appearing and evolving intra-articular alterations (inside the joint). Generally, what happens is that the muscles, being hypertonic, lose their capacity to synchronize the displacement of the meniscus or articular disc with the movements of the mandibular condyle inside the fossa or glenoid cavity of the temporal bone.
2- Disc Displacement WITH Reduction (Click)
This ailment occurs when (with the mouth closed) the disc is not in its correct position, on top of the condyle facing the fossa, but in a more anterior position. As a consequence, as soon as the jaw begins to open, the condyle encounters an obstacle to its movement and slows down. If the opposite joint is normal, the mouth appears to open with a deviation to the affected side.
At a certain point, the opening push overcomes the elastic resistance of the disc and the condyle jumps forward, repositioning itself under the disc with a typical sound known as a “click”. Looking at the patient, we can then observe that the jaw, which had a deviation of trajectory, straightens the course instantly.
From this point on, the jaw follows a perfectly straight opening path.
As the patient closes his mouth, he follows a path that is reversed in such a way that, almost at the same point where the disc had been “recaptured”, it is “lost” again with a symmetrically opposite click and jump to those of the opening. In this case, the click is called “reciprocal” (both on opening and closing).
If the affected condyles are both (right and left), the mandible will emit two reciprocal clicks at the joints, and its trajectory will mark an “S” shape.
3- Disc Displacement WITHOUT Reduction (Blocking)
As in the previous case, in this situation the disc is in front of the condyle when it is in rest position with the mouth closed. The difference is that as soon as the jaw begins its opening path, the condyle cannot recover the disc, so there is no reduction (no “click”).
It happens that the disc curls elastically in front of the condyle and prevents it from advancing. The result is that the patient then presents a limit of movement in the affected part, the jaw makes a deviated opening towards the blocked side and the opening width, as a whole, is shorter than normal.
This condition is often after a period in which the affected TMJ clicked and is determined by anterior disc slippage. In blocking, two subdivisions are possible:
- Acute The patient has a click, suddenly he can no longer perceive it and instantly falls into a blocking condition.
- Chronic The patient has a long-term reduced movement and may have developed some adaptation.
4- Disc-Ligament Compression
In all those situations in which the disc is not in its correct position, the condyle rests on a structure that is not normally involved: the posterior ligament of the articular meniscus. This anatomical structure is rich in blood vessels and nerves, which makes jaw movements painful due to continuous friction on its sensitive parts and the formation of fluid bubbles inside the joint capsule. Sometimes, a sound can be heard (crepitus) similar to rubbing with sand or rolling a newspaper, due to contact between the bone surfaces.
This specific type of temporomandibular disorder usually becomes chronic, with alternating phases of acute symptoms and remissions. A possible evolutionary result is the deformation of the condyle with the formation of arthrosis.
5- Articular Disc Perforation or Fracture
The disc or meniscus has a fibrotic structure and its excessive thinning, due to the continuous destructive changes in the joint, can result in a perforation, which can occur in the posterior insertion tissue or inside the body of the meniscus without reduction. This can alter the internal hydrodynamic action of the synovial fluid and predispose it to fracture. The fracture of the disc implies its fragmentation and complete separation.
As in the previous case, crepitus is a clinical indication of meniscal perforation, or at least of its posterior insertion. Crepitus, sometimes called crepitation, describes any grinding, creaking, cracking, grating, crunching, or popping that occurs when moving a joint. Noise is an indicator of direct friction between two bone surfaces.
6- Degenerative TMJ Disorder (Osteoarthritis)
Temporomandibular joint osteoarthritis is a unilateral degenerative disease of the lower jaw joint. It is characterized by the breakdown of the articular cartilage, architectural changes in the bone and degeneration of the synovial tissues; causing a picture of severe pain, dysfunction and functional disability that affects nutritional, social and health parameters.
A disorder of this developmental level completely prevents opening the mouth and chewing.
Etiology and Possible Causes of Gnathological Dysfunction
Temporomandibular disorders are one of the most intriguing and controversial topics in the world of Dentistry. In particular, its etiology has been a subject of intense debate for many years.
Despite all the technological advances in the diagnostic sciences, no conclusive and unanimous agreement has yet been reached on the etiology of these disorders. Ancient researchers looked for only a somatogenous cause, however, current research shows that psychological and social factors also play an important role. The only certainty is that it is a pathology of multifactorial origin.
It is not yet clear if some of these causes lead directly to TMJ syndrome or if they are the result of the disorder. General causes can include genetics, jaw injuries, poor posture, personality and behavior, stress or anxiety level, arthritis, infections, autoimmune diseases and other musculoskeletal inflammatory disorders.
Among the most frequent dental causes we find:
- Malocclusions In many cases, the closed position of the two dental arches (occlusion) can cause a postural problem in the mandible, being compensated by asymmetric muscular tensions. To make dental gear possible and comfortable, the muscles are forced to work incorrectly. The most frequent problems are premature contacts, interferences, occlusal instability and loss of vertical dimension.
- Clenching It is the habit of the patient to keep the teeth in permanent and very tight contact, continually forcing the closing muscles (temporal and masseter, mainly).
- Bruxism It is the custom of rubbing or grinding the teeth with force, making sliding movements in all directions and generating a very characteristic noise. In many cases, this habit has a non-dental origin, for example, the stress of the patient’s daily life. The results are a series of signs and symptoms such as tooth abrasion, coronal fractures and muscle aches; among many others.
- Bad Habits A classic example is compulsive use of chewing gum. It forces the muscles to work uselessly for hours, with all the consequences already described.
Exploration and Diagnosis of TMDs
The primary approach to diagnosing temporomandibular disorders is clinical. First, it is based on a series of tests and observations that help distinguish whether the problem is articular or muscular. A correct sequence of analysis will allow, in the vast majority of cases, to correctly categorize the patient’s complaint.
However, it must be said that in recent years diagnostic protocols have become much more precise, leaving many of the criteria that were applied in the past without effect.
One of the most relevant current resources is what is now considered the most important instrumental diagnostic tool in Gnathology: magnetic resonance imaging (MRI). As with all the joints of the body, this exam is the only one that agrees to visualize a very important element of the TMJ: the articular disc or meniscus.
This latter, in fact, is not visible in any X-ray image, a circumstance that denotes the relative uselessness of panoramic radiographs in the study of these pathologies. In addition, MRI offers the advantage of allowing unlimited repetitions of the study, since they do not emit ionizing radiation and are not harmful to the patient.
By combining both the clinical examination and the MRI, we will be able to formulate a correct diagnosis and suggest an appropriate treatment.
Conservative Gnathological Therapy
Temporomandibular disorders, obviously, have different approaches depending on the diagnosis. The principles are assimilable to orthopedic and physiotherapeutic criteria, so we are talking about procedures aimed at articular reconditioning, muscle relaxation therapies and devices with orthopedic functions for the bite correction (splints or mouth guards).
The first step will always be to rule out any genetic malformation, severe trauma, or systemic disease. Next, perform an occlusal (bite) analysis, eliminate any premature contact or occlusal interference using selective grinding techniques, and provide indications for home care.
Splints deserve a special mention, because when faced with a gnathological disorder, they are usually indicated immediately, almost as a reflex action. The detail lies in the fact that there exist many types of splints, with different designs and properties, for which the clinician must be prepared and know which one is the most indicated according to the characteristics and peculiarities of the case. They could even be contraindicated in some circumstances.
So if the diagnosis is not accurate, the generic application of “a splint” will not solve much. Within a modern approach, it is the combination of various techniques and resources that leads to the most appropriate solution:
- Mandibular Exercises These are a set of specific exercises and movements indicated to try to regain functional balance and get relief from classic articular problems (clicks). Its goal is to get the maximum possible muscular relaxation, through some stretching maneuvers. It is like yoga for the mouth.
- Neuromuscular Bite It is a transparent acrylic plate that is applied on a dental arch (generally the upper one), making the teeth rest on a different surface, specifically created. It has some aspects in common with the old concept of the “plane of the bite”, although unlike this, it is conceived with a reduced lingual size and more precise lateral guides. Its main objectives are to relax the muscles and protect the patient’s teeth.
- Mandibular Repositioning Bite It is a special splint used specifically in the treatment of the displacement of the disc with reduction. It is placed in the upper arch and has an internal ramp that forces the lower jaw to close in an advanced position, to facilitate the recapture of the meniscus.
- Distraction Bite This splint is constructed in the lower dental arch with a premature contact on one side only, this to force the patient to bite towards the other. It is used in cases of compression of the posterior ligament and then it is adjusted until symptomatic improvement is achieved, after which it is reconverted into a neuromuscular bite.
- Orthodontics Once the case has been stabilized and the patient is symptom-free, it is very likely that the Gnathologist will indicate a corrective orthodontic treatment if he or she observes obvious malocclusion or misaligned teeth. A good occlusion or bite, with good dental gear during chewing, is the ideal environment to prevent masticatory dysfunctions and temporomandibular disorders.
“Gnathology Is the Dental Specialty that Treats Mandibular Problems Through the Study of the Biology of the Masticatory System and Temporomandibular Joint”.
DENTAL TIP
Other Treatment Options
In some incipient cases, the symptoms of temporomandibular joint disorders may disappear thanks to conservative treatments, including occlusal splints, selective grinding, medication with muscle relaxants, anti-inflammatories and psychotropics; psychotherapy, physiotherapy, different mandibular bio-feedback techniques and orthodontics.
But if your symptoms persist or if your case is very advanced, it will be necessary to resort to other treatment options, often applying more than one at a time:
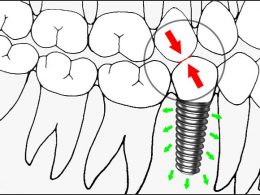
- Oral Rehabilitation The replacement of lost teeth in cases of multiple edentulous spaces and obvious alteration of the functional occlusal pattern, is usually indicated to generate new engrams, reestablish disocclusion patterns and improve the neuromuscular condition of the patient. In addition, dental crowns or onlays may be necessary to modify the position or height of severely malpositioned teeth.
- Infiltrations In some people, corticosteroid injections into the joint can be helpful. In others, injecting botulinum toxin type A (Botox) into the masticatory muscles can relieve pain associated with TMJ disorders.
- Arthrocentesis and Joint Lavage It consists of the aspiration of fluid from the interior of the joint cavity and the injection of a therapeutic substance. In essence it is a minimally invasive surgical intervention that induces the joint to function and adapt itself.
- TMJ Arthroscopy In some cases, arthroscopic surgery can be as effective in treating various types of TMJ disorders as open joint surgery. A small thin tube (cannula) is placed into the articular space, then an arthroscope is inserted and small surgical instruments are used for surgery. TMJ arthroscopy has fewer risks and complications than open joint surgery, but it also has some limitations.
- Modified Condylotomy The modified condylotomy addresses the TMJ indirectly, with an osteotomy at the level of the mandibular condyle. Its theoretical basis is supported by the conviction that by modifying the condyle, the muscles that are inserted into it will passively reposition themselves and promote a more favorable relationship between the condyle, the disc and the fossa.
- Open Surgery If your jaw pain does not resolve with any of the above treatments because your joint has osteoarthritis or irreversible damage, your Gnathologist or Maxillofacial Surgeon may suggest open joint surgery (arthrotomy) to repair or rebuild it. However, open joint surgery carries more risks than other procedures and should be considered very carefully, only after discussing the pros and cons of the intervention.
Come to Venezuela and Forget About Removable Dentures!
Never forget that dental tourism is an extraordinary tool for accessing top-notch Dentistry.
DENTAL VIP trusts that quality of dental care should be affordable to all, no matter where you live. Hundreds of patients come to Venezuela for state-of-the-art medical and dental care every year, saving large amounts of money on health. Our rates are significantly lower than in any other Latin American country (up to 70% off), without it implying a decrease or compromise in the quality of service. Our Professional Staff is one of the best in the country and has extensive experience in dental and zygomatic implants, metal-free crowns and bridges, oral rehabilitation, smile design and cosmetic dentistry.
We guarantee that by using the services offered by DENTAL VIP, you will be cared for in modern facilities, with state-of-the-art equipment and under the standards of the most demanding international dental protocols.
Come for the price and stay for the quality! Contact us today through WhatsApp +58 414-9033547 or Email and we will let you know, according to your case, all the evaluations and basic studies required for your treatment.