Table of Contents
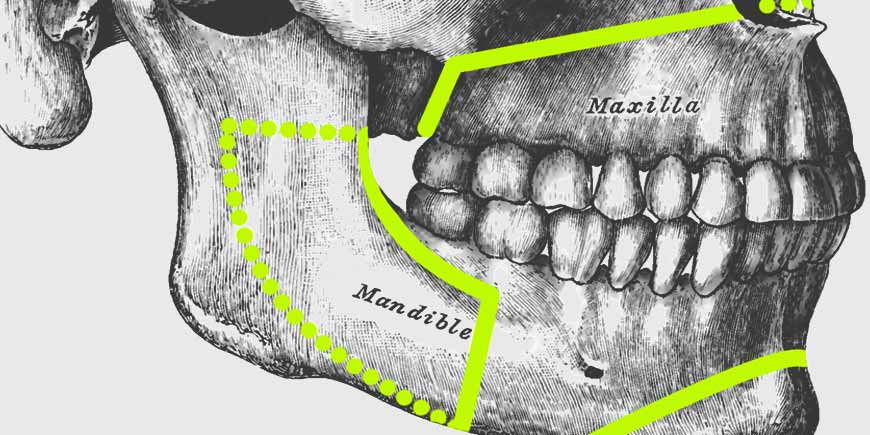
The jawbones differ from other bones in the body in several ways. Embryologically, they are unique, because they develop from cells that migrate from the embryonic neuroectoderm. Anatomically, they house teeth and dental germs, elements totally unrelated to their histological structure. With both unique characteristics, diseases occur in them that are not seen in any other part of the skeleton.
For the purposes of this topic, these will be divided into 2 main groups: those related to dentition and those restricted to the bone itself. Diseases of the jawbones associated with teeth can be divided into odontogenic cysts and tumors. Reactive bone diseases, fibro-osseous lesions, giant cell lesions, and other bone tumors; will be described in the second part of this post.
Similarly, both benign entities (non-neoplastic) and malignant pathologies (neoplastic) will be addressed and analyzed.
What Is the Difference Between a Cyst and a Tumor?
Cysts and tumors are two different pathological entities:
- Cyst A cyst is a sac that can be filled with air, fluid, or other material. It can form anywhere in the body, including bones, organs, and soft tissues. Most cysts are not malignant, but they can sometimes be caused by neoplasms.
- Tumor A tumor is an abnormal mass of body tissue. Like cysts, a tumor can form anywhere in the body. A tumor can be benign or malignant (cancerous).
The best test to determine whether a cyst or tumor is benign or malignant, is a biopsy. This procedure involves removing a sample of the suspicious tissue or, in some cases, the entire lesion; to study it under microscopy.
Odontogenic Cysts
Most cysts in the jawbones are called odontogenic, as they derive from the odontogenic epithelium that is related to the formation and development of teeth. Only a few are non-odontogenic, since they derive from another type of embryonic tissue, different from the one that gives rise to the teeth.
Odontogenic cysts are classified as inflammatory and developmental. In the first group, inflammatory changes are the stimulus for the odontogenic epithelial remnants to proliferate and transform into epithelium-lined cystic cavities. This means that its appearance may be related to poor oral health. Proper dental care reduces its incidence.
The most common inflammatory odontogenic cysts are:
- Radicular Cysts They are located at the tips or apices of the roots of the teeth with necrotic pulp tissue, mainly due to extensive untreated caries.
- Paradental Cysts They have the same histological characteristics as radicular cysts, but they are located in the lateral portion of the root, between the enamel and the root cement. It is believed that they may be related to deep periodontal sacs.
- Residual Cysts They are radicular or paradental cysts that remain in the maxilla after the extraction of the associated teeth.
The pathogenesis of developmental odontogenic cysts is not well understood, but it is known that they originate in the germ structures of the tooth and are classified according to the stages of odontogenesis (process of embryonic formation of teeth) in which they are produced.
- Dentigerous Cysts They surround the crown of a non-erupted tooth. These cysts can be oversized and radiologically they can be confused with odontogenic tumors.
- Lateral Periodontal Cysts They are found between the roots of vital teeth. This distinguishes them from radicular cysts, which are associated with non-vital teeth.
- Gingival Cysts The adult gingival cyst is a rare type of cyst that is made up of soft gingival tissue. It can form on free or attached gingiva.
- Glandular Odontogenic Cyst Also called sialo-odontogenic cyst, it is a rare developmental odontogenic cyst. The most common mode of presentation is a slowly growing intraosseous lesion in the anterior part of the mandible, most often crossing the midline.
- Odontogenic Keratocyst The most frequent location is in the area of the lower third molar, at the level of the mandibular angle, from where they progress towards the ramus and the body. Its importance lies in its high recurrence rate located between 30 and 60%. Odontogenic keratocysts constitute about 19% of mandibular cysts.
Non-Odontogenic Cysts
As the name already implies, these cysts are not related to the tissues that make up the teeth.
- Nasopalatine Duct Cyst This cyst is found in the anterior portion of the palate, just behind the upper central incisors. Its coating consists of a mixture of squamous and respiratory epithelium.
- Nasolabial Cyst The nasolacrimal duct is the one that usually gives rise to this type of lesion. This cyst forms in the soft tissue of the buccal aspect of the alveolar process, just next to the nose. Due to its location in soft tissues, it is difficult to detect radiographically.
Odontogenic Tumors
Odontogenic tumors comprise a group of lesions that have in common the fact that they arise from the odontogenic tissues (which make up the teeth). Because dental germs have an epithelial and a mesenchymal part, these tumors can be epithelial, mesenchymal, or mixed.
Clinically, this group of growths includes entities whose behavior varies from frankly neoplastic (malignant), including metastatic potential, to non-neoplastic hamartomatous lesions (of benign growth). These last can simulate normal tooth development, including the formation of hard dental tissues such as enamel, dentin, and cementum.
It is obvious that an accurate diagnosis is mandatory, on the one hand to avoid unnecessary overtreatment in case of benign growth lesions, and on the other, to avoid delays in the treatment of genuine neoplasms. Due to the overlapping histological features, this is not always easy. Let us see the most common odontogenic tumors:
- Epithelial Tumors Among those with the highest incidence we find: desmoplastic tumors and unicystic ameloblastomas, calcifying epithelial odontogenic tumor, adenomatoid odontogenic tumor and squamous odontogenic tumor.
- Mesenchymal Tumors Mainly myxomas, fibromas and cementoblastomas.
- Mixed Odontogenic Tumors Mixed odontogenic tumors contain both epithelial and mesenchymal tissues and can mimic odontogenesis to varying degrees. When the lesion resembles the germ of an immature tooth, without the presence of dentin or enamel, it is called ameloblastic fibroma. If they consist entirely of a mixture of dentin and enamel, they are called odontomas. Two other common tumors of this type are the calcifying cystic odontogenic tumor and the ghost cell odontogenic tumor.
- Malignant Tumors Malignant odontogenic tumors, also called primary intraosseous carcinomas, are very rare neoplasms, are located mainly in the mandible and originate by direct extension of an adjacent primary tumor into the oral cavity; or are metastatic deposits of distant primary lesions. The best known are ameloblastic carcinoma, ameloblastic fibrosarcoma, ameloblastic fibrodentinosarcoma, and ameloblastic fibroodontosarcoma.
Reactive Bone Lesions
Reactive bone lesions present in 2 different forms. The first is the so-called torus. These lesions are bony outgrowths of the cortical bone. They are mostly found in the mid-palatal line, buccally on the maxillary alveolar ridge, or lingually on the mandibular alveolar ridge.
The second group that is considered under this denomination are infectious and inflammatory diseases. The presence of oral infections may represent a gateway for the microorganisms that cause infection of the jawbone. If bone necrosis and pus formation predominate, it is referred to as acute osteomyelitis.
Fibro-Osseous Lesions
Fibro-osseous lesions are characterized by the presence of bone marrow that has become fibrous tissue and contains mineralized material of variable appearance, sometimes similar to dental tissue. Their current classification recognizes fibrous dysplasia, ossifying fibroma, and cemento-osseous dysplasia.
- Fibrous Dysplasia It presents in three clinical subtypes: monostotic that affects one bone, polyostotic that affects multiple bones, and Albright’s syndrome in which multiple bone lesions are accompanied by skin hyperpigmentation and endocrine abnormalities.
- Ossifying Fibroma It can affect both the mandible and the maxilla. This bone tumor consists of highly cellular fibrous tissue that contains varying amounts of calcified tissue that resembles bone, cementum, or both. This injury can be mistaken for an osteosarcoma.
- Cemento-Osseous Dysplasia It occurs in 4 different clinical forms. Periapical cemento-osseous dysplasia that manifests itself predominantly in the anterior region of the mandibular bone, at the periapical level of the incisors and canines. Focal cemento-osseous dysplasia, which occurs in the molars and premolars; and florid cemento-osseous dysplasia, which is more extensive and involves two or more quadrants of the bone. The latter is also known by the name of multiple gigantiform cementoma, especially when it is highly expandable and involves multiple quadrants.
Giant Cell Lesions
Central giant cell granuloma of the jaws is a relatively common disease. It is locally aggressive and presents as a soft tissue mass with different clinical and histological characteristics whose etiology, pathogenesis and therapy; have not been clearly defined.
This type of lesion represents 6.6% of all maxillary tumors. It is one of the most frequently encountered expandable lesions. It affects population groups in early and advanced ages, and between the second and third decade of life. It occurs in both sexes, and more frequently in women, in a 2:1 ratio.
Other Non-Odontogenic Bone Tumors
Like any other bone in the body, the jawbones can eventually be affected by benign and malignant, primary and metastatic tumors, which have nothing to do with the teeth (non-odontogenic tumors).
Tumoral growths of cartilage, bone, connective, lymphatic, hematopoietic and vascular tissue; are possible in the maxillofacial region. Logically, its description goes beyond the objectives of this post.
Diagnostic Procedure
When detecting the existence of any of these lesions, the first thing to do is not to waste time. The finding is usually made during a routine dental visit or by the sudden appearance of some increase in volume within the orofacial region.
To collect more information about your maxillary cyst or tumor, we may recommend some tests that may include imaging studies (such as X-rays, CT scans, or magnetic resonances) and, in many cases, a biopsy; to extract a sample of the tissue of the lesion and make a histopathological study.
If the problem is only of dental origin and is within your expectations, our Dentists and Surgeons will develop a treatment plan to eliminate your cyst or tumor. If, on the contrary, the lesion is very large, shows clinical signs of malignancy or is supposed to be associated with some systemic compromise, we will immediately refer you to the best multidisciplinary medical team in our city.
“In the Face of the Sudden Appearance of Any Mass or Abnormal Growth of Tissue in the Orofacial Region, the Most Important Thing Is Not to Waste Time and Go Immediately to the Doctor or Dentist”.
DENTAL TIP
Treatment Options
Treatment options for jaw cysts and tumors vary depending on the type of lesion, its evolutionary stage, and its clinical signs and symptoms.
In some cases it is not necessary to intervene, just observe the lesion and make sure it does not evolve. In others, treating the teeth that caused the problem will suffice. However, the treatment of jaw cysts and tumors, generally involves a surgical intervention. In addition, treatment may include the participation of a multidisciplinary medical team.
During surgery, surgeons remove the jaw cyst or tumor, which may also include the removal of teeth, healthy tissue, and bone; to achieve a clean or safe surgical margin and remove any neoplastic cell that may have infiltrated into apparently healthy tissue.
Next, a Pathologist examines the extracted tissue and reports a histopathological diagnosis, on which the continuity and evolution of the treatment will depend.
Other cases may include reconstruction of the jaw or other anatomical structures, oncologic therapy for certain types of cysts and tumors (chemotherapy and radiotherapy), and supportive care to help maintain quality of life; including assistance with nutrition, speech, and swallowing.
If the lesion was extensive or very aggressive, it is usually necessary to replace or substitute teeth, so Prosthodontics is, sometimes, part of the general treatment plan.
As is logical, if the tumor was malignant, a life-long control and follow-up is essential, to avoid recurrences, or in the worst of cases; treat them on time.
Ready to Finally Get the Dental Treatment You Deserve?
All you have to do is send us your dental basic studies so that our professional team can analyze your case and offer you the best treatment option, many times impossible to pay in your home country.
Lower pricing does not always mean reduced quality. DENTAL VIP Specialists are trained in the most modern dental techniques, and we are equipped with state-of-the-art instruments.
We will offer the best price at the best quality for you in dental implants, All on 4, crowns and bridges, oral surgery, zygomatic implants, aesthetic dentistry, endodontics, full mouth reconstruction and other highly specialized treatments.
If you are considering coming to Venezuela for dental work, contact us for more information on how we can help you.
Our WhatsApp Business contact +58 414-9033547 and our email info@dentalvipcaracas.com are at your absolute and complete disposal to make inquiries and provide you with the best possible guidance in Dentistry.