Table of Contents
Because dental implants are more susceptible to occlusal overloading issues, in comparison to natural teeth, ideal implant occlusion is of paramount importance for oral function and the prevention of implant-related complications.
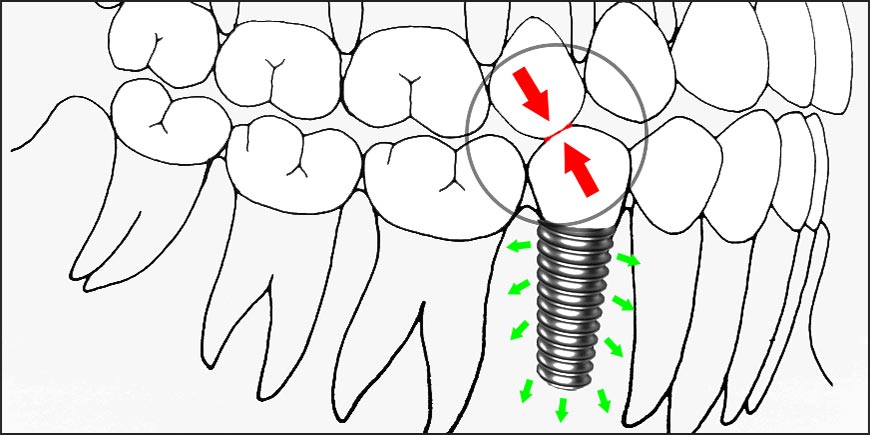
After rigid fixation of the dental implant is achieved (osseointegration), the health of the associated hard and soft tissues is dependent on the mechanical stress and strain from occlusal loading or masticatory forces. Thus, a primary cause of peri-implantitis and bone loss around implants is the excessive force applied from unwanted occlusal contacts.
Additionally, mechanical complications such as screw loosening and fractures, as well as prosthesis and implant fracture, may also occur from occlusal overload. In this post we will see how teeth and implants differ in response to occlusal stress and some specific recommendations for occlusion for single, partial and full-arch implant prostheses.
Differences Between Teeth and Dental Implants
A natural tooth is suspended by a periodontal ligament (PDL), which allows for axial displacement (between 25–100 micrometers), while an endosseous implant has a bony interface with minimal axial displacement (between 3–5 micrometers).
The PDL surrounding a natural tooth is functionally oriented for axial loads, allowing for physiological-functional adjustments in response to excessive occlusal stresses. Additionally, the PDL will allow for adaptation to jaw deformation and torsion in the natural teeth. In contrast, dental implants lack the supportive PDL mechanism and will deflect in a linear and elastic pattern, which is totally dependent on the elastic deformation of the supporting bone.
Implants Are Susceptible to Force-Related Issues
Studies have shown that mechanical stress or strain beyond the physical limits of hard tissues is a primary cause of bone loss around loaded implants. The PDL present around natural teeth contains periodontal mechanoreceptors, which play a key role in the sensory discriminative capabilities and control of jaw function.
These neurophysiological receptors transmit information from the nerve endings on the magnitude, direction and rate of occlusal load for sensory perception and neuromotor control. Therefore, patients are usually aware when natural teeth are in hyperocclusion, which usually results in sensitivity and pain.
After tooth loss, these intra-dental and periodontal mechanoreceptors become necrotic and resorb, resulting in the loss of fine proprioceptive control. Thus, implants, which lack the advantages of the PDL associated with teeth, are highly susceptible to occlusal overload.
Effects of Non-Axial (Horizontal) Forces
There exist three types of forces placed on dental implants from occlusal loading: compressive, tensile and shear. Bone is strongest in compression and weakest in shear. Most forces from mastication are not vertical, but are horizontal (non-axial).
When non-vertical loading occurs on natural teeth, they adapt more favorably than dental implants. Studies have shown that lateral forces on a healthy natural tooth are rapidly dissipated away from the bone crest toward the apex of the tooth. A dental implant, however, will not pivot or rotate; therefore, the non-vertical stress will most likely result in trauma to the supporting bone. The stress will cause bone microfractures, resulting in eventual bone loss or mechanical failure of the prosthetic components.
Implant-Protected Occlusion
The concept of implant-protected occlusion (IPO) was developed by Dr. Carl Misch for prosthetic rehabilitation with dental implants. The goal of IPO is to reduce the biomechanical stress to the implant interface and the prosthesis.
The ideal occlusal scheme for an implant prosthesis is designed to control the stress on the implant system, provide a prosthetic and biologically acceptable implant interface, and maintain long-term stability of the marginal bone, soft tissue and prosthesis.
The IPO principles address several conditions to decrease stress to the implant system, including existing occlusion, implant body angle to occlusal load, cusp angle of implant crowns, occlusal table width, mutually protected articulation, cantilever or offset loads, crown contour, occlusal contact position, and timing of occlusal contacts.
Recommendations for Single and Partial Implant Prostheses
The goal of implant-protected occlusion for a single implant crown or bridge is to minimize occlusal overload. We consider that all clinicians should incorporate the next principles into their implant restorations to maintain forces within physiologic limits and to provide long-term stability of the implant system, including the restorative material, abutment screws and cement retaining the structures.
- Implant Positioning Ideally, the implant body should be positioned perpendicular to the curves of Wilson and Spee to minimize the possibility of non-axial, angled forces. Ideal positioning of the implants within the bone is vitally important to minimize stress to the implant system.
- Maintain Narrow Posterior Occlusal Table The width of the occlusal table should be directly proportional to the implant body diameter. Normally, a 30–40 percent reduction in the occlusal table is recommended. In some instances, the opposing tooth may require recontouring of a cusp to help direct the occlusal force along the long axis of the implant body.
- Minimal Posterior Cusp Inclination Increased cusp inclination of the implant crowns will most likely result in an angled load to the implant body. The occlusal contact along any of the angled cusps results in a non-axial force vector. Therefore, the clinician should adhere to a more shallow, or monoplane, cusp height, which will decrease force-related complications.
- No Premature Contacts On Implant Crowns A premature contact occurs when an occlusal contact interferes with the normal movement and positioning of the mandible upon closure. Premature contacts, or hyperocclusion, may cause bone loss or implant failure, therefore; the occlusion should always be meticulously evaluated on a continuous basis, and irregular and malpositioned cusps should be modified on the opposing dentition for a more favorable force distribution.
- Ideal Occlusal Contact Position Occlusal contact position determines the direction of force, which, if not ideal, may be detrimental to the peri-implant hard and soft tissues. When anterior implants are being restored, whenever possible, only the natural teeth should be utilized as the stress-bearing component of the occlusal scheme to prevent overstressing the implant prosthesis. In the posterior region, the occlusal contact should be on a flat surface perpendicular to and within the diameter of the implant body, which directs axial forces within the central fossa.
- Timed Occlusal Contacts Ideally, natural teeth should exhibit greater initial contacts in comparison to implants through timing of the contacts. The goal of timed occlusal contacts is to eliminate the mobility differences between teeth and implants. This will allow for an even distribution of occlusal load and prevention of premature contacts and increased loads.
- Increased Proximal Contact Area The broader contacts will establish a greater surface area to distribute forces between the implants and the adjacent natural teeth. This is also important to avoid food impaction, formation of black triangles, caries and periodontal defects.
- Mutually Protected Articulation When posterior teeth are in contact, the forces are directed along the long axis of the implants, reducing forces on and contact between the anterior teeth. During lateral and protrusive movements, no posterior occlusal contacts should be present, as the forces are directed to the anterior teeth.
Recommendations for Fixed Full-Arch Implant Prostheses
In the literature, fixed full-arch implant restorations have been shown to have many advantages over removable or conventional prostheses, including greater masticatory force and efficiency, higher satisfaction rates, less maintenance, greater bone maintenance and superior prosthesis success rates.
With the evolution of modern implantology, edentulous patients have the opportunity to improve their quality of life and benefit from the advantages of a fixed full-arch implant prosthesis. However, controlling and maintaining occlusion is imperative in reducing mechanical and biological complications, thus increasing the longevity of the prosthesis.
They can be metal-porcelain or hybrid. The hybrid ones consisting of a metal substructure with denture teeth and acrylic, to replicate the soft tissue. Regardless of the type of prosthesis, it is essential to always consider the following aspects to achieve a successful treatment:
- Ideal Implant Position With a full-arch prosthesis, there exist key implant positions that are crucial to reduce force. The two most important positions are the canine and first molar, as both the magnitude and direction of the force is increased at these arch positions. Additionally, an implant positioned in the incisor area should be considered to minimize an anterior cantilever effect.
- Increased Implant Surface Area Ideally, the implant surface area, which includes the number of implants and diameter of the implant bodies, should be increased, especially when the opposing occlusion is natural teeth or there exist parafunctional habits. A prosthesis with compromised implant surface area will lead to increased stress and strain, and possible biomechanical overload.
- Minimized Cantilevers Because of the pneumatization of the maxillary sinus and mandibular posterior bone loss, cantilevers are often utilized in full-arch implant prostheses to replace the first molar in the maxilla or mandible. Cantilever bridges are dental bridges that are designed when abutment teeth are prepared on only one side of the missing toothless gap. In such cases, the pontic is located outside the abutment teeth. They act as force magnifiers, and their presence will lead to tensile forces, which increase the stress on the implants and the prosthesis. The destructive nature of cantilevers has been shown to result in peri-implant bone loss and prosthesis failure.
- Shallow Anterior Guidance With a fixed full-arch implant prosthesis, the anterior guidance should remain shallow. The steeper the incisal guidance, the greater the resultant force on the anterior segment. Some studies stated that for every 10-degree increase in incisal guidance, a 30 percent increase in force to the anterior segment will result. Additionally, increased anterior guidance will result in a higher possibility of posterior contacts, which lead to greater muscle activity.
- Occlusal Pattern Currently, there are no controlled studies on the ideal occlusion for fixed full-arch implant prostheses. Thus, there exists no accepted consensus on the ideal occlusal scheme for patients. At DENTAL VIP, the experience of many years has led us to implement the pattern of bilateral balanced occlusion only when the other arch is restored with a conventional denture, group function when the implant is located at the level of the canines or lateral incisors and mutually protected occlusion when the full-arch implant restoration opposes an arch with natural dentition or that is restored with a fixed implant prosthesis or an implant-supported overdenture.
“The Health of the Bone that Fixes and Retains the Implants, Will Always Depend on the Chewing Forces, the Occlusal Load and the Mechanical Tension to Which They Are Exposed”.
DENTAL TIP
Occlusal Guard
With an implant-supported prosthesis, there exists no protective feedback system (proprioception), leading to biting forces that are greater in comparison to those exerted by natural dentition. Additionally, patients are less aware of premature contacts, which may result in biomechanical overload. All patients with dental implants will benefit from an occlusal guard, especially if parafunctional habits are present.
At DENTAL VIP we always recommend the use of this type of device at night, to sleep, in all those patients who present occlusal dysfunction, parafunctional habits, extensive conventional restorations or prostheses over dental implants. To our knowledge, an occlusal discharge splint constitutes a kind of “life insurance” for oral rehabilitations.
To End…
For oral function and the prevention of dental-implant-related complications, ideal implant occlusion is of the utmost importance. In order to properly treatment plan an implant case, clinicians must have an understanding of the fundamental differences between teeth and dental implants with respect to occlusal loading forces.
Due to biomechanical differences between teeth and implants, modifications must be made in the development of occlusal schemes for prosthetic rehabilitation. The topic of dental implant occlusion is very complex; therefore, the clinician must take into consideration many factors in the formulation of an occlusal scheme for each specific type of prosthesis.
Hence the importance of multidisciplinary treatment in oral implantology. Surgery and Prosthetics are two completely different Specialties, and it is very difficult for the same Dentist to master both. For dental implants you do not need a Dentist, you need a team, a Team of Specialists. Always remember it!
We Are Just One Step Away!
Globalization and Dental Tourism are two extraordinary tools for accessing world-class dentistry. Currently millions of people travel to other countries in search of opportunities and prices that allow them to face their dental treatments and recover their smile.
Wherever you are, generally in just a few hours you will be able to get to Venezuela, move to a comfortable hotel and start your Oral Rehabilitation process with Dental Implants, Porcelain Veneers and 100% Metal-Free Ceramic Structures; at only a fraction of the cost you would have to pay in your home country.
Almost certainly traveling or not traveling will mean the difference between satisfaction and resignation, or at best; between just getting “something” or be able to reach “the best option”. At DENTAL VIP we are very good hosts and excellent professionals.
Contact us and ascertain how traveling to Venezuela can improve your self-esteem and quality of life!